NRNP 6645: Cognitive Behavioral Therapy in a Comparative Context
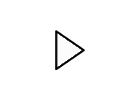
 Cognitive Behavioral Therapy (CBT) is a well-established psychotherapy approach that has proven highly effective in treating a variety of mental health disorders, including anxiety, depression, PTSD, substance use disorders, and more (Impala et al., 2022).
Cognitive Behavioral Therapy (CBT) is a well-established psychotherapy approach that has proven highly effective in treating a variety of mental health disorders, including anxiety, depression, PTSD, substance use disorders, and more (Impala et al., 2022).
In nursing, CBT is commonly used to help patients understand and modify the cognitive distortions and negative thought patterns that influence their emotions and behaviors.
This technique is essential in Psychiatric Nursing and CBT as it equips nurses to better manage mental health challenges.
Research has consistently shown that CBT can be more effective than other therapeutic methods, making it an integral part of CBT in Nursing and CBT for Mental Health Professionals.
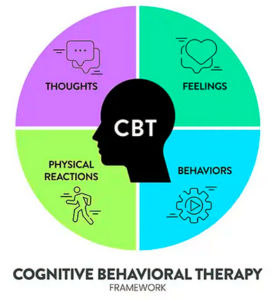
CBT focuses on changing thought patterns to improve emotional responses and behaviors. It is frequently used in a variety of settings, such as CBT for Anxiety, Depression, and PTSD, and also in treating CBT for Substance Use Disorders. However, its application varies across individual, family, and group therapy formats.

Struggling to meet your deadline?
Get your assignment on NRNP 6645: Cognitive Behavioral Therapy in a Comparative Context done by certified MDs and PhDs in the USA. ORDER NOW!
CBT in Nursing Practice
In Psychiatric Nursing, CBT is utilized to enhance patient outcomes by focusing on the connection between thoughts, feelings, and behaviors. It is especially beneficial in CBT for Mental Health Professionals and CBT in Psychiatric Nursing Practice, as it allows nurses to tailor interventions to meet the unique needs of patients with mental health disorders. Through Evidence-Based Practice in CBT, psychiatric nurses can address cognitive distortions and work with patients to develop more adaptive coping strategies, improving adherence to treatment plans and overall mental well-being.
Different Approaches to CBT: Individual, Group, and Family
Individual CBT involves one-on-one sessions between a therapist and patient. This setting allows for a personalized approach, where the therapist works directly with the patient to identify distorted thinking patterns and replace them with healthier alternatives (Feldman, 2013). This can be especially effective for Psychiatric Nurse Practitioner and CBT, as it gives the practitioner the space to develop a tailored therapeutic relationship with the patient.
In Group Therapy Techniques in Nursing, group CBT is often used in settings where multiple patients share similar issues. Group CBT can be a cost-effective alternative to individual sessions, providing social support while encouraging accountability and shared learning among participants (Fogarty et al., 2019). Group therapy in Psychiatric Nursing and CBT is particularly useful for conditions like anxiety or depression, where patients benefit from learning coping strategies together and sharing experiences.
Family CBT focuses on the family unit, addressing the impact of family dynamics on the mental health of individuals. In this approach, the therapist works with family members to recognize and alter unhealthy cognitive patterns that contribute to family stress or conflict (Feldman, 2013). This type of therapy can be beneficial in Cognitive Behavioral Therapy for Families, helping families communicate more effectively and resolve conflicts.
Challenges in Implementing CBT
While CBT is highly effective, there are challenges in implementing it, especially in Group CBT and Family CBT settings. For example, in CBT for Psychiatric Nursing, nurses may face difficulties in managing group dynamics, such as members feeling uncomfortable sharing personal issues. In family therapy, therapists may encounter resistance from family members who are either not motivated to participate or who have pre-existing negative patterns that hinder progress (Ringle et al., 2015). These challenges highlight the need for specialized strategies in Integrating CBT into Nursing Care Plans.
Challenges in Group CBT also arise when the group size is too large, limiting the therapist’s ability to address each individual’s concerns in detail (Psych Exam Review, 2019). Additionally, negative emulation can occur in group settings, where patients may unintentionally adopt harmful behaviors from others, such as in cases of substance use or eating disorders (Sochting, 2014).
Overcoming Challenges in Group CBT requires strategies like small group sizes, clear guidelines for participation, and regular feedback. Nurses can overcome challenges by fostering a supportive and non-judgmental environment that encourages open communication and trust.
Evidence-Based Benefits of CBT in Nursing
The integration of CBT in Nursing Practice is supported by substantial evidence demonstrating its effectiveness in improving mental health outcomes, including better symptom management and treatment adherence. Research indicates that CBT for Anxiety, Depression, and PTSD significantly reduces the severity of these conditions and helps patients develop healthier coping mechanisms (Impala et al., 2022). In CBT for Substance Use Disorders, studies have shown that CBT helps individuals recognize triggers for substance use and develop strategies for avoiding relapse.
Moreover, CBT for Mental Health Professionals is essential for enhancing the skill set of Psychiatric Nurse Practitioners (PMHNP), ensuring they can implement evidence-based interventions that improve patient outcomes. This is why CBT for Nurses is critical in developing the necessary competencies for advanced psychiatric practice.
Key Benefits of CBT for PMHNPs
The use of CBT can significantly improve the therapeutic relationship between PMHNPs and their patients. By using CBT in Psychiatric Nursing Practice, PMHNPs can help patients challenge and reframe negative thought patterns, which are crucial in treating mental health disorders. This leads to better Patient Adherence and more effective Mental Health Interventions for Nurses.
CBT and Treatment Outcomes in Nursing
The role of CBT in improving treatment outcomes is well-documented. CBT and Patient Adherence is particularly important, as it helps patients remain engaged in their treatment plans and improves their overall mental health status. This can be achieved through consistent practice and support from nurses who are trained in CBT for Nurses and Psychiatric Nurse Practitioner and CBT.
In Individual and Group CBT for Nursing Students, education on these approaches prepares future nurses to apply CBT in clinical settings, enhancing their ability to treat a wide range of psychiatric conditions.
Conclusion
CBT is a powerful therapeutic tool in Psychiatric Nursing that can be applied in individual, group, and family settings. While challenges exist, especially in terms of group dynamics and patient resistance, CBT in Nursing provides evidence-based solutions to address these obstacles. By integrating CBT into nursing care plans and utilizing it to enhance communication and treatment adherence, nurses can significantly improve the mental health outcomes of their patients. With ongoing research and Evidence-Based Practice in CBT, the future of CBT in Nursing Practice looks promising, offering valuable interventions for patients across various mental health conditions.
References
- Feldman, L. B. (2013). Integrating individual and family therapy. Routledge.
- Fogarty, C., Hevey, D., & McCarthy, O. (2019). Effectiveness of cognitive behavioural group therapy for social anxiety disorder: Long-term benefits and aftercare. Behavioural and Cognitive Psychotherapy, 47(5), 501-513.
- Impala, T., Okamoto, A., & Kazantzis, N. (2023). Alliance rupture and repair in cognitive behavior therapy. In C. F. Eubanks, L. W. Samstag, & J. C. Muran (Eds.), Rupture and repair in psychotherapy: A critical process for change (pp. 119–139). American Psychological Association.
- Ringle, V. A., et al. (2015). Barriers to and facilitators in the implementation of Cognitive-Behavioral Therapy for youth anxiety in the community. Psychiatric services, 66(9), 938–945.
- Sochting, I. (2014). Cognitive Behavioral Group Therapy: Challenges and Opportunities. Wiley & Sons Ltd.
NRNP 6645: Cognitive Behavioral Therapy in a Comparative Context.
Cognitive behavioral therapy (CBT) represents a mode of psychotherapy that has garnered substantial evidence of its effectiveness in addressing a broad spectrum of mental health conditions, encompassing anxiety disorders, issues related to alcohol and drug use, marital conflicts, eating disorders, and severe mental health conditions (Impala et al., 2022). Extensive research has demonstrated the superior efficacy of CBT when contrasted with alternative psychotherapeutic approaches. CBT equips individuals with the capacity to identify and rectify distorted or pessimistic thought patterns, allowing them to perceive challenging circumstances with greater clarity and respond to them with increased efficacy. However, CBT exhibits variation in its application, with distinctions among group, individual, and family therapy settings.
Mastering Med Surg: A Guide to Success
Group Cognitive Behavioral Therapy
Group CBT focuses on administering therapy to a collective of individuals grappling with similar issues. These groups can serve as both a source of support and a platform for the exchange of ideas (Fogarty et al., 2019). Frequently, fellow group members collaborate to generate concrete solutions for surmounting difficult situations or life challenges, providing mutual accountability along the way. This group dynamic not only functions as a support system but also presents a cost-effective alternative compared to one-on-one sessions (Fogarty et al., 2019).
Individual Cognitive Behavioral Therapy
Individual CBT constitutes a form of psychotherapy concentrating on the influence of thoughts and mental imagery on an individual’s emotions and behaviors (Feldman, 2013). The process commences with orientation, followed by the establishment of a therapeutic relationship and a shared commitment to achieving positive outcomes. Therapists often tailor their strategies to align with the specific needs of each patient. As the therapeutic relationship evolves, the therapist systematically identifies troubling circumstances, fosters emotional awareness, and addresses and reshapes negative or distorted thought patterns.
Family Cognitive Behavioral Therapy
Family CBT represents an approach within CBT that places the family unit at its core, based on the premise that family members exert mutual influence on one another, sometimes leading to detrimental feedback loops. The principal objective of this approach is to facilitate family members’ recognition of cognitive distortions, subsequently reconfiguring their thought processes and modifying behavior to enhance their interpersonal dynamics (Feldman, 2013). In family therapy, the therapist diligently examines cognitive behavioral patterns within the family, drawing from individual and joint interviews, self-report questionnaires, and observations of family interactions.
Challenges in Implementing CBT
CBT, while effective, presents its own set of challenges, driving therapists to continually develop strategies to address these issues. In group CBT, one prominent challenge pertains to group dynamics, as members may hold differing perspectives (Sochting, 2014). For instance, in a video by the “Beck Institute for Cognitive Behavior Therapy” (2018, June 7), the therapist illustrated how a husband and wife may view their marriage from distinct angles. In such cases, the therapist focuses on facilitating changes within the individuals’ control, such as how they interpret each other’s behaviors.
Another challenge arises in the context of Family CBT, where some family members may lack motivation. Factors such as diverse socioeconomic backgrounds, low educational attainment, poverty, and disruptive behaviors can impact motivation negatively and disrupt the group therapy process (Ringle et al., 2015). To address this challenge, therapists must encourage members to acknowledge their accomplishments, break down tasks into manageable steps, and identify positive experiences throughout their day.
References
Feldman, L. B. (2013). Integrating individual and family therapy. Routledge.
Fogarty, C., Hevey, D., & McCarthy, O. (2019). Effectiveness of cognitive behavioural group therapy for social anxiety disorder: Long-term benefits and aftercare. Behavioural and Cognitive Psychotherapy, 47(5), 501-513. DOI: 10.1017/S1352465819000079
Impala, T., Okamoto, A., & Kazantzis, N. (2023). Alliance rupture and repair in cognitive behavior therapy. In C. F. Eubanks, L. W. Samstag, & J. C. Muran (Eds.), Rupture and repair in psychotherapy: A critical process for change. (pp. 119–139). American Psychological Association. https://doi.org/10.1037/0000306-006Links to an external site.
Ringle, V. A., Read, K. L., Edmunds, J. M., Brodman, D. M., Kendall, P. C., Barg, F., & Beidas, R. S. (2015). Barriers to and Facilitators in the Implementation of Cognitive-Behavioral Therapy for Youth Anxiety in the Community. Psychiatric services (Washington, D.C.), 66(9), 938– 945. https://doi.org/10.1176/appi.ps.201400134Links to an external site.
Sochting, I. (2014). Cognitive Behavioral Group Therapy: Challenges and Opportunities. Wiley & Sons Ltd
COGNITIVE BEHAVIORAL THERAPY: COMPARING GROUP, FAMILY, AND INDIVIDUAL SETTINGS
There are significant differences in the applications of cognitive behavior therapy (CBT) for families and individuals. The same is true for CBT in group settings and CBT in family settings. In your role, it is essential to understand these differences to appropriately apply this therapeutic approach across multiple settings. For this Discussion, as you compare the use of CBT in individual, group, and family settings, consider challenges of using this approach with groups you may lead, as well as strategies for overcoming those challenges.
RESOURCES
Be sure to review the Learning Resources before completing this activity.
Click the weekly resources link to access the resources.
To prepare:
- Review the videos in this week’s Learning Resources and consider the insights provided on CBT in various settings.
BY DAY 3
Post an explanation of how the use of CBT in groups compares to its use in family or individual settings. Explain at least two challenges PMHNPs might encounter when using CBT in one of these settings. Support your response with specific examples from this week’s media and at least three peer-reviewed, evidence-based sources. Explain why each of your supporting sources is considered scholarly and attach the PDFs of your sources.
Read a selection of your colleagues’ responses.
Exploration of Cognitive Behavioral Therapy (CBT) Across Different Settings
Cognitive Behavioral Therapy (CBT), as elucidated by Wheeler (2020), operates on the fundamental principle that one’s mental well-being hinges on their ability to adapt cognitively and functionally to environmental changes by rectifying behaviors influenced by cognitive distortions and assumptions through behavioral experiments. CBT is distinguished by its problem-focused approach, which involves pinpointing specific areas necessitating solutions, and its action-oriented nature, which centers on reconfiguring behaviors and mindsets to achieve more favorable outcomes (Psych Exam Review, 2019).
When CBT is applied within group settings, it aims to address individuals’ concerns collectively. In this context, therapists engage with participants to assess, diagnose, and treat symptoms while imparting coping skills and facilitating behavioral changes. Group CBT leverages the advantage of mutual learning, as individuals facing similar problems and challenges within the group can draw upon one another’s experiences to resolve issues and identify behaviors that require adjustment (Psych Exam Review, 2019). Group therapy, besides its educational benefits, also presents a cost-effective alternative to individual therapy, making it more accessible and time-efficient for therapists who can cater to multiple patients concurrently.
CBT’s utility extends to couples, where it serves as a vehicle for enhancing problem-solving skills, effective communication, conflict resolution, and addressing issues such as sexual dysfunction, domestic violence, and the art of fair verbal disagreements without resorting to harmful tactics (Nichols, 2022).
In the realm of family therapy, CBT revolves around the dynamics of familial relationships and treats the family unit as a whole. The approach in family therapy emphasizes behavioral training, implementing reward and consequence systems to teach family members constructive communication, emotional management, and the modification of distressing behaviors.
Challenges Encountered in CBT Settings
In group CBT, therapists confront the challenge of potential negative emulation. Participants with shared problems may inadvertently pick up harmful coping strategies from one another. An illustrative example is evident when the presenter discussed how individuals in a Bulimia nervosa group might learn new techniques for purging and concealing their actions, or individuals who engage in self-harm may acquire fresh methods to hide their wounds (Psych Exam Review, 2019).
Furthermore, group size poses another obstacle for therapists in group CBT settings. Larger groups may hinder the therapist’s ability to comprehensively address each member’s concerns. Some individuals might not feel comfortable speaking up about their issues, and time constraints can prevent in-depth exploration of all the challenges faced due to the sheer volume of participants (Psych Exam Review, 2019).
It is worth noting that CBT remains a collaborative process between the therapist and the patient, serving as an effective approach for imparting skills to modify behaviors, alleviate symptoms, enhance treatment adherence, and sustain therapeutic progress (Kopelovich & Tarkington, 2021).
References
Nichols, M., & Davis, S. (2020). Basic Techniques of Family Therapy. The essentials of family therapy (7th ed.). pp. 23–39. Pearson.
Kopelovich, S. L., & Turkington, D. (2021). Remote CBT for Psychosis During the COVID-19 Pandemic: Challenges and Opportunities. Community Mental Health Journal, 57(1), 30–34. https://doi.org/10.1007/s10597-020-00718-0
Wheeler, K. (2020). Psychotherapy for the Advanced Practice Psychiatric Nurse (3rd ed.). Springer Publishing LLC. https://mbsdirect.vitalsource.com/books/9780826193896
PsychExamReview. (2019, April 30). Cognitive therapy, CBT, & group approaches (intro psych tutorial #241)
BY DAY 6 OF WEEK 1
Respond to at least two of your colleagues by recommending strategies to overcome the challenges your colleagues have identified. Support your recommendation with evidence-based literature and/or your own experiences with clients.
Note: For this Discussion, you are required to complete your initial post before you will be able to view and respond to your colleagues’ postings. Begin by clicking on the Reply button to complete your initial post. Remember, once you click on Post Reply, you cannot delete or edit your own posts and you cannot post anonymously. Please check your post carefully before clicking on Post Reply!
Discussing the Utilization of Cognitive Behavioral Therapy (CBT) Across Different Contexts
Cognitive Behavioral Therapy (CBT), as described by Wheeler (2020), is a guided therapeutic approach predicated on the belief that mental health is intricately linked to an individual’s capacity to adapt positively, both cognitively and functionally, to changes in their environment. This adaptation involves the modification of behaviors influenced by cognitive distortions and assumptions, achieved through the implementation of behavioral experiments. CBT is characterized by its problem-oriented nature, emphasizing transparency in identifying specific areas necessitating solutions and its action-oriented approach, which involves the reconfiguration of behaviors and mindsets to attain more favorable outcomes (Psych Exam Review, 2019).
When CBT is employed within a group setting, it serves as a means to collectively address the issues faced by individuals. Within this context, therapists engage with participants, assessing, diagnosing, and treating symptoms while imparting coping skills and facilitating the adoption of new behaviors as a catalyst for change. Group CBT offers the distinct advantage of mutual learning, as individuals within the group, sharing common problems and needs, can glean insights from one another’s experiences, understand how to overcome issues, and identify behaviors that require adjustment (Psych Exam Review, 2019). Group therapy presents an additional advantage in terms of cost-effectiveness, making it a more financially accessible option compared to individual therapy. Moreover, it optimizes the therapist’s time, allowing them to accommodate multiple patients within the same time frame as an individual session.
CBT in couples serves to educate partners in enhancing their problem-solving skills, effective communication, conflict resolution, and addressing issues such as sexual dysfunction, domestic violence, and engaging in fair verbal disagreements without resorting to harmful tactics (Nichols, 2022).
In the realm of family therapy, CBT centers on the dynamics of familial relationships, treating the family unit as a holistic system. Family CBT emphasizes behavioral training, implementing a system of rewards and consequences to instill healthy modes of communication, emotional management, and the modification of distressing behaviors among family members.
Challenges Faced by PMHNPs in CBT Settings
In a group CBT session, therapists may encounter the challenge of negative emulation. Members of the group who share similar problems may inadvertently acquire detrimental techniques for handling their issues from one another. An example is evident when the presenter discussed individuals in a Bulimia nervosa group potentially learning new methods to purge and conceal their actions or individuals who engage in self-harm discovering fresh strategies to conceal their self-inflicted wounds (Psych Exam Review, 2019).
Another challenge therapists may face in group settings is the potential inability to address all members’ issues comprehensively. This challenge arises due to the group’s size, making it challenging for every participant to voice their concerns or allowing insufficient time to delve into all the issues presented because of the large number of participants (Psych Exam Review, 2019).
It is essential to recognize that CBT operates as a collaborative process between the therapist and the patient, serving as an effective method for teaching skills to modify behaviors, alleviate symptoms, bolster treatment adherence, and maintain therapeutic progress (Kopelovich & Tarkington, 2021).
References
Nichols, M., & Davis, S. (2020). Basic Techniques of Family Therapy. The essentials of family therapy (7th ed.). pp. 23–39. Pearson.
Kopelovich, S. L., & Turkington, D. (2021). Remote CBT for Psychosis During the COVID-19 Pandemic: Challenges and Opportunities. Community Mental Health Journal, 57(1), 30–34. https://doi.org/10.1007/s10597-020-00718-0
Wheeler, K. (2020). Psychotherapy for the Advanced Practice Psychiatric Nurse (3rd ed.). Springer Publishing LLC. https://mbsdirect.vitalsource.com/books/9780826193896Links to an external site.

Dont wait until the last minute.
Provide your requirements and let our native nursing writers deliver your assignments ASAP.