NUR 502 Week 3 Pulmonary Function DR and Ms Brown Case Study St Thomas University
 D.R. is a 27-year-old man, who presents to the nurse practitioner at the Family Care Clinic complaining of increasing SOB, wheezing, fatigue, cough, stuffy nose, watery eyes, and postnasal drainage—all of which began four days ago.
D.R. is a 27-year-old man, who presents to the nurse practitioner at the Family Care Clinic complaining of increasing SOB, wheezing, fatigue, cough, stuffy nose, watery eyes, and postnasal drainage—all of which began four days ago.
Three days ago, he began monitoring his peak flow rates several times a day.
His peak flow rates have ranged from 65-70% of his regular baseline with nighttime symptoms for 3 nights on the last week and often have been at the lower limit of that range in the morning.
Three days ago, he also began to self-treat with frequent albuterol nebulizer therapy. He reports that usually his albuterol inhaler provides him with relief from his asthma symptoms, but this is no longer enough treatment for this asthmatic episode.

Struggling to meet your deadline?
Get your assignment on NUR 502 Week 3 Pulmonary Function DR and Ms Brown Case Study St Thomas University done by certified MDs and PhDs in the USA. ORDER NOW!
Case Study Questions
- According to the case study information, how would you classify the severity of D.R. asthma attack?
- Name the most common triggers for asthma in any given patients and specify in your answer which ones you consider applied to D.R. on the case study.
- Based on your knowledge and your research, please explain the factors that might be the etiology of D.R. being an asthmatic patient.
Fluid, Electrolyte and Acid-Base Homeostasis
Ms. Brown is a 70-year-old woman with type 2 diabetes mellitus who has been too ill to get out of bed for 2 days. She has had a severe cough and has been unable to eat or drink during this time. On admission, her laboratory values show the following:
• Serum glucose 412 mg/dL
• Serum sodium (Na+) 156 mEq/L
• Serum potassium (K+) 5.6 mEq/L
• Serum chloride (Cl–) 115 mEq/L
•Arterial blood gases (ABGs): pH 7.30; PaCO2 32 mmHg; PaO2 70 mmHg; HCO3– 20 mEq/L
Case Study Questions
- Based on Ms. Brown admission’s laboratory values, could you determine what type of water and electrolyte imbalance does she has?
- Describe the signs and symptoms to the different types of water imbalance and described clinical manifestation she might exhibit with the potassium level she has.
- In the specific case presented which would be the most appropriate treatment for Ms. Brown and why?
- What the ABGs from Ms. Brown indicate regarding her acid-base imbalance?
- Based on your readings and your research define and describe Anion Gaps and its clinical significance.
Submission Instructions:
- You must complete both case studies
- Your initial post should be at least 500 words per case study, formatted and cited in current APA style with support from at least 2 academic sources. Your initial post is worth 8 points.
- You should respond to at least two of your peers by extending, refuting/correcting, or adding additional nuance to their posts. Your reply posts are worth 2 points (1 point per response.)
- All replies must be constructive and use literature where possible.
- Please post your initial response by 11:59 PM ET Thursday, and comment on the posts of two classmates by 11:59 PM ET Sunday.
- You can expect feedback from the instructor within 48 to 72 hours from the Sunday due date.
Pulmonary Function
NUR 502 Week 3 Pulmonary Function DR and Ms Brown Case Study St Thomas University
In accordance with the information provided in the case study, how would you categorize the severity of D.R.’s asthma attack?
Based on the case study, D.R.’s asthma is categorized as moderate persistent asthma, which is defined by daily symptoms such as coughing, wheezing, chest tightness, or shortness of breath, and significant interference with normal activities. In D.R.’s case, symptoms occur daily, including nighttime symptoms five or more times a month, as well as a FEV 1 ranging from 65-70% of normal values, indicating that the lung function is moderately impaired. Additionally, the patient’s peak flow monitoring for asthma shows a greater than 30% variability, which indicates poor asthma control. This scenario requires asthma management with asthma medication (e.g., albuterol, corticosteroids) to alleviate symptoms and prevent further exacerbation (Bush, 2019).
Asthma Severity Classification and Management
Asthma severity classification is essential for effective asthma management. In D.R.’s case, the moderate persistent asthma classification guides treatment, which should include daily controller medications like inhaled corticosteroids and rescue medications like albuterol for acute symptoms. This also involves regular use of peak flow monitoring for asthma to assess lung function and ensure timely intervention during an asthma exacerbation. D.R. must be educated on recognizing worsening symptoms and when to seek emergency treatment.
Treatment strategies include optimizing medication use, reducing exposure to asthma triggers, and ensuring proper asthma patient education to manage symptoms effectively. Patient education is crucial for improving asthma self-management practices and enhancing quality of life. Additionally, addressing any potential environmental triggers for asthma (such as allergens or irritants) is key to preventing exacerbations.
Common Triggers of Asthma and Their Impact on D.R.
Common triggers for asthma include environmental allergens (e.g., dust mites, animal fur, pollen), irritants such as tobacco smoke, household sprays, and paint fumes, along with viral infections, exercise, and stress (Chau-Etchepare et al., 2019). For D.R., a viral respiratory infection seems to be a major factor in triggering the asthma exacerbation. The patient presents with symptoms of a cold, including postnasal drainage and watery eyes, which may have worsened the asthma symptoms. Recognizing these asthma triggers is important for preventing further attacks. D.R. should be educated on avoiding viral infections and managing exposure to environmental triggers for asthma like mold, pets, and dust mites.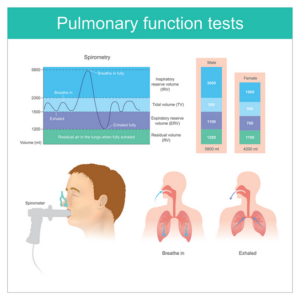
Factors Contributing to D.R.’s Asthma Diagnosis
Several factors may contribute to D.R.’s asthma diagnosis. Genetic factors are significant, as asthma has a strong familial component. Asthma pathophysiology suggests that inherited genes related to airway inflammation and bronchial hyperresponsiveness play a role in disease development. D.R. may have inherited these genetic variations from family members with a history of asthma (Chau-Etchepare et al., 2019).
Environmental triggers for asthma, such as exposure to dust mites, animal allergens, or mold, may also be contributing factors, especially if D.R. lives in an environment with these allergens. Additionally, work-related asthma may be a concern if D.R. is exposed to irritants at work. Occupational asthma is common in jobs involving chemicals, cleaning products, or dust (Chau-Etchepare et al., 2019). A combination of these genetic and environmental factors likely led to D.R.’s diagnosis of asthma, emphasizing the importance of chronic asthma care and asthma self-management.
Fluid, Electrolyte, and Acid-Base Imbalances in a Diabetic Patient
As we look at electrolyte imbalance in diabetes, it’s crucial to note that patients with diabetes are at risk for both hypernatremia and hypokalemia, especially during acute illnesses or diabetic ketoacidosis (DKA). Acid-base disturbances in diabetes, such as metabolic acidosis, can exacerbate these imbalances, leading to dangerous complications. In elderly diabetic patients, fluid resuscitation is particularly important, as they may have reduced kidney function and be more prone to dehydration and electrolyte imbalances (Chau-Etchepare et al., 2019).
Electrolyte Imbalances in Diabetes: Focus on Hypernatremia and Hyperkalemia
Hypernatremia treatment and hypokalemia are common concerns in diabetic patients. These imbalances can result from dehydration, poor kidney function, or complications of diabetic ketoacidosis (DKA). Hyperkalemia can occur in cases of acute kidney injury, often seen in poorly controlled diabetes. ABG interpretation in diabetes is essential to assess the severity of these imbalances, helping clinicians decide on the appropriate treatment strategy, which may involve fluid resuscitation and careful monitoring of electrolytes.
Acid-Base Disturbances in Diabetic Patients: ABG Interpretation
ABG (arterial blood gas) interpretation in diabetes is essential when diagnosing acid-base disturbances. Diabetic ketoacidosis (DKA) leads to metabolic acidosis, characterized by low bicarbonate levels and an elevated anion gap. This can be life-threatening if not treated promptly. Understanding the anion gap clinical significance helps clinicians assess the degree of acidosis and determine the necessary fluid resuscitation and electrolyte management, particularly for patients with type 2 diabetes mellitus management issues.
Clinical Manifestations of Electrolyte Imbalances in Elderly Patients
Elderly patients with diabetes are particularly vulnerable to electrolyte imbalances due to age-related changes in kidney function and the body’s ability to regulate fluid and electrolyte balance. Electrolyte imbalances in diabetes may manifest as weakness, confusion, irregular heartbeat, or muscle cramps. Given the age-related risks, careful monitoring of electrolytes and timely interventions like fluid resuscitation are crucial. Nursing assessments should regularly include checks for signs of hypokalemia or hyperkalemia in elderly diabetic patients.
Treatment Strategies for Managing Electrolyte Imbalances in Diabetic Patients
Managing electrolyte imbalances in diabetes involves a combination of fluid resuscitation, monitoring of ABG values, and the correction of hypernatremia and hypokalemia through intravenous fluids or oral supplements. In cases of diabetic ketoacidosis (DKA), treatment must focus on reversing the acidosis, replenishing electrolytes, and managing blood sugar levels. This requires a multi-faceted approach to stabilize the patient’s condition and prevent further complications, such as acid-base disturbances in diabetes.
Understanding the Anion Gap and Its Clinical Significance
The anion gap clinical significance is crucial for evaluating acid-base disturbances in diabetic patients, particularly in the context of diabetic ketoacidosis (DKA). An elevated anion gap indicates metabolic acidosis, a common complication of DKA. Understanding this value helps in determining the appropriate treatment, which may involve fluid resuscitation and careful management of electrolytes. Correct interpretation of ABG results, along with the patient’s clinical symptoms, is essential for managing these conditions.
Conclusion: Integrating Asthma and Diabetes Care
In managing D.R., both asthma management and diabetes management must be considered holistically. For moderate persistent asthma, appropriate asthma medication (e.g., albuterol, corticosteroids) and asthma self-management strategies are essential.
Simultaneously, monitoring and managing electrolyte imbalances in diabetes, especially in the context of diabetic ketoacidosis and acid-base disturbances in diabetes, is critical for overall patient health. Regular monitoring of peak flow and ABG interpretation for both conditions will help guide the treatment plan and prevent complications in D.R.’s care. Education on both asthma patient education and diabetic care will ensure better outcomes and improve D.R.’s quality of life.
References
Bush, A. (2019). Pathophysiological Mechanisms of Asthma. Frontiers in pediatrics, pp. 7, 68. https://doi.org/10.3389/fped.2019.00068
Chau-Etchepare, F., Hoerger, J. L., Kuhn, B. T., Zeki, A. A., Haczku, A., Louie, S., Kenyon, N. J., Davis, C. E., & Schivo, M. (2019). Viruses and non-allergen environmental triggers in asthma. Journal of investigative medicine: the official publication of the American Federation for Clinical Research, 67(7), 1029–1041. https://doi.org/10.1136/jim-2019-001000
Qian, Q. (2019). Hypernatremia. Clinical journal of the American Society of Nephrology: CJASN, 14(3), 432–434. https://doi.org/10.2215/CJN.12141018
Quade, B. N., Parker, M. D., & Occhipinti, R. (2021). The therapeutic importance of acid-base balance. Biochemical Pharmacology, 183, 114278. https://doi.org/10.1016/j.bcp.2020.114278
Wu, Y., Fu, Y. Y., Zhu, H. D., Xu, J., & Walline, J. H. (2022). Treatment of hyperkalemic emergencies. World journal of emergency medicine, 13(3), 232–236. https://doi.org/10.5847/wjem.j.1920-8642.2022.054

Dont wait until the last minute.
Provide your requirements and let our native nursing writers deliver your assignments ASAP.

