NURS 6501 Advanced Pathophysiology: Alterations in Cellular Processes
 This paper aims to explain the pathophysiology of cystic fibrosis, focusing on the genetic basis, cellular dysfunction, and nursing implications of the disease.
This paper aims to explain the pathophysiology of cystic fibrosis, focusing on the genetic basis, cellular dysfunction, and nursing implications of the disease.
Cystic fibrosis is a chronic, inherited disorder that affects multiple organ systems, especially the lungs, pancreas, and gastrointestinal tract.
The disease is caused by mutations in the CFTR gene on chromosome 7, leading to defective chloride transport across epithelial membranes, resulting in thick and sticky mucus.
This impairs the functioning of several organs, including the lungs, pancreas, and intestines. The nursing implications of cystic fibrosis are profound, as managing the symptoms and providing patient education are crucial for improving the quality of life and outcomes.
Nurses must understand the genetic basis of cystic fibrosis and be familiar with cystic fibrosis patient care, including treatment options such as enzyme replacement therapy, and CFTR gene mutation therapies. This paper will explore how nursing professionals can use research findings and advanced practice strategies in cystic fibrosis care plans to manage the disease effectively.

Struggling to meet your deadline?
Get your assignment on NURS 6501 Advanced Pathophysiology: Alterations in Cellular Processes done by certified MDs and PhDs in the USA. ORDER NOW!
Genetics and the CFTR Gene
The genetic basis of cystic fibrosis lies in mutations of the CFTR gene, which codes for the CFTR protein. This protein plays a critical role in transporting chloride ions across epithelial membranes. When the CFTR gene is mutated, it results in CFTR protein dysfunction, leading to impaired chloride transport, cellular dehydration, and the accumulation of thick mucus in various organs. This dysfunction explains the common symptoms observed in cystic fibrosis, such as gastrointestinal dysfunction cystic fibrosis, failure to thrive cystic fibrosis, and salty skin cystic fibrosis. The disease is inherited in an autosomal recessive pattern, meaning both parents must carry a defective copy of the CFTR gene for their child to inherit the disease.
The CFTR gene mutation is most commonly associated with a deletion of three base pairs in the gene’s sequence, leading to the absence of phenylalanine at position 508 (ΔF508). The understanding of this genetic mutation CFTR protein is essential for developing targeted therapies. CFTR gene mutation therapies are currently a key area of research, aiming to correct the malfunctioning CFTR protein to improve chloride transport and reduce symptoms. For nursing professionals, it is crucial to stay updated on the latest nursing research regarding genetic treatments, as these advancements will significantly influence the management and outcomes of cystic fibrosis. 
Cellular Mechanisms in Cystic Fibrosis
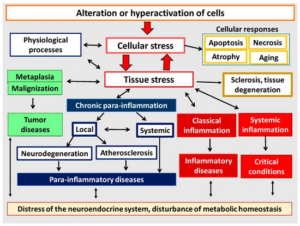
Cystic fibrosis involves a cellular dysfunction in cystic fibrosis, where the defective CFTR protein causes a breakdown in chloride transport within epithelial cells. This defect leads to an imbalance in sodium and chloride ions, resulting in water retention in the cells. The result is thickened mucus, which obstructs ducts in the lungs, pancreas, and gastrointestinal tract. The impaired ion transport disorder cystic fibrosis affects cellular hydration, which causes cellular dehydration in cystic fibrosis. In the lungs, this thick mucus leads to chronic respiratory infections and airway obstruction, while in the digestive system, it causes pancreatic insufficiency in cystic fibrosis, leading to malabsorption of essential nutrients. These issues are compounded by chronic inflammation and cell death, or apoptosis, which are direct consequences of the defective CFTR protein’s effects on epithelial cells.
The malfunction of the CFTR protein in cystic fibrosis is responsible for the failure to thrive cystic fibrosis observed in children. Poor nutrient absorption results in stunted growth and low body weight, often requiring interventions like enzyme replacement therapy to aid in digestion. Understanding the pathophysiological mechanisms at the cellular level is critical for developing effective treatment plans for patients, especially when considering nursing assignments that require deep insights into the molecular mechanisms of diseases like cystic fibrosis.
Symptoms of Cystic Fibrosis in Children
In children, cystic fibrosis presents with a variety of symptoms of cystic fibrosis in children that reflect the dysfunction of multiple organs. One of the most distinctive symptoms is salty skin cystic fibrosis, due to the inability to reabsorb chloride ions in the sweat glands. This leads to elevated levels of salt in the sweat, which is often used as a diagnostic marker. Other common symptoms include gastrointestinal dysfunction cystic fibrosis, such as bloating, poor appetite, and foul-smelling stools due to pancreatic insufficiency in cystic fibrosis. This results from the inability of the pancreas to secrete sufficient digestive enzymes, leading to malabsorption of nutrients, poor weight gain, and failure to thrive cystic fibrosis.
Respiratory symptoms, including chronic cough, wheezing, and recurrent lung infections, are also common in cystic fibrosis patients. The buildup of thick mucus in the lungs leads to airway obstruction and creates an environment conducive to bacterial growth, resulting in frequent infections. Understanding the pathophysiology of cystic fibrosis is vital for managing these symptoms and guiding appropriate nursing interventions. Nurses working with cystic fibrosis patients must be prepared to address both the physical and emotional challenges that children with the disease and their families face. This often involves using online nursing papers and resources to stay up to date on the latest evidence-based practices in cystic fibrosis patient care.
Pathophysiological Responses in Cystic Fibrosis
The pathophysiology of cystic fibrosis is driven by the genetic mutation CFTR protein and its impact on chloride transport. This mutation causes a cascade of cellular responses, including thickened mucus production, airway obstruction, chronic inflammation, and tissue damage. The ion transport disorder cystic fibrosis leads to impaired water and electrolyte balance across epithelial cells, which ultimately results in the dehydration of cellular surfaces and the formation of viscous mucus that cannot be cleared. This causes cellular dehydration in cystic fibrosis, which significantly impacts the lungs, gastrointestinal system, and pancreas.
These pathophysiological responses explain many of the classic symptoms of cystic fibrosis, such as difficulty breathing, frequent respiratory infections, and malnutrition due to pancreatic insufficiency in cystic fibrosis. Gastrointestinal dysfunction cystic fibrosis can also cause liver disease, bile duct obstruction, and malabsorption of vitamins, all of which worsen the patient’s quality of life. For nurses, understanding these pathophysiological responses is essential for developing targeted interventions and providing effective care to individuals with cystic fibrosis.
Nursing Implications and Treatment
 The nursing implications of cystic fibrosis are vast, as the disease requires ongoing management and monitoring. Nurses play a crucial role in ensuring that patients with cystic fibrosis receive appropriate treatments for gastrointestinal dysfunction cystic fibrosis and respiratory issues. One important aspect of treatment is enzyme replacement therapy, which helps patients with pancreatic insufficiency in cystic fibrosis digest and absorb nutrients. Nurses must educate patients and their families about the importance of maintaining a high-calorie diet, managing medications, and incorporating airway clearance techniques into daily routines.
The nursing implications of cystic fibrosis are vast, as the disease requires ongoing management and monitoring. Nurses play a crucial role in ensuring that patients with cystic fibrosis receive appropriate treatments for gastrointestinal dysfunction cystic fibrosis and respiratory issues. One important aspect of treatment is enzyme replacement therapy, which helps patients with pancreatic insufficiency in cystic fibrosis digest and absorb nutrients. Nurses must educate patients and their families about the importance of maintaining a high-calorie diet, managing medications, and incorporating airway clearance techniques into daily routines.
As part of the nursing care plan, nurses must also be familiar with CFTR gene mutation therapies, which aim to correct the genetic defect that underlies cystic fibrosis. These therapies are currently in clinical trials and are showing promise in improving the function of the CFTR protein and alleviating symptoms. Nurses can support patients and families in understanding the potential benefits of these treatments, which may include newer medications that target the defective gene directly.
Nursing research continues to play a critical role in improving cystic fibrosis care. Nurses involved in online nursing research have access to a wealth of information regarding the latest treatments, clinical trials, and patient care strategies. By keeping up with top nursing essays, custom nursing papers, and nursing assignments, nurses can improve their understanding of cystic fibrosis and enhance patient outcomes.
Cystic Fibrosis Treatment Options
Treatment options for cystic fibrosis are multifaceted, aiming to manage the disease’s symptoms and slow its progression. Traditional treatments include enzyme replacement therapy for pancreatic insufficiency, antibiotics to control lung infections, and airway clearance techniques to help patients expel thick mucus. Newer therapies, such as CFTR gene mutation therapies, have been developed to target the underlying genetic defect and improve the function of the CFTR protein. These therapies are providing significant improvements in lung function and quality of life for many cystic fibrosis patients.
For nursing professionals, it is important to stay informed about the latest cystic fibrosis treatment options. This often involves reviewing online nursing essays, nursing exams, and academic papers that discuss the latest clinical guidelines and treatment innovations. Nurses can also benefit from engaging in nursing assignments that explore the application of these therapies in real-world clinical settings, providing better care to patients with cystic fibrosis.
Conclusion: Advancements in Cystic Fibrosis Care
In conclusion, cystic fibrosis remains a complex disease with a wide range of symptoms and complications. However, significant advancements in CFTR gene mutation therapies, enzyme replacement therapy, and nursing research have led to better management and improved outcomes for patients. Nursing implications of cystic fibrosis are critical in providing holistic care that addresses both the physical and emotional aspects of living with the disease. Nurses must stay up to date with the latest evidence-based practices and leverage resources such as online nursing papers, nursing exams, and best nursing papers to continue improving care for patients with cystic fibrosis.
By understanding the underlying genetic basis of cystic fibrosis, the cellular mechanisms in cystic fibrosis, and the available treatment options, nurses can play a vital role in managing this challenging disease and supporting families through their journey. Advancements in cystic fibrosis care will continue to improve the lives of those affected, and nurses will remain at the forefront of this progress, using their knowledge and skills to make a lasting difference.
To prepare:
By Day 1 of this week, you will be assigned to a specific scenario for this Discussion. Please see the “Course Announcements” section of the classroom for your assignment from your Instructor.
By Day 3 of Week 1
Post an explanation of the disease highlighted in the scenario you were provided. Include the following in your explanation:
The role genetics plays in the disease.
Why the patient is presenting with the specific symptoms described.
The physiologic response to the stimulus presented in the scenario and why you think this response occurred.
The cells that are involved in this process.
How another characteristic (e.g., gender, genetics) would change your response.
Read a selection of your colleagues’ responses.
By Day 6 of Week 1
Respond to at least two of your colleagues on 2 different days and respectfully agree or disagree with your colleague’s assessment and explain your reasoning. In your explanation, include why their explanations make physiological sense or why they do not
Introduction to Cellular Functions and Disease Mechanisms
Cells are indeed the fundamental building blocks of the body, each with a specific function that contributes to the overall physiological operations necessary for health. The concept of cellular specialization—where cells perform distinct roles according to their structure—directly ties into the central dogma of molecular biology, which explains how genes orchestrate these specialized cellular functions. This process is fundamental for maintaining normal bodily functions. However, as you rightly point out, when disease intervenes, it disrupts the normal functioning of cells, causing alterations in their structure and functions, which can lead to pathological conditions. The exploration of diseases, including the case of sore throat related to allergic conditions, offers valuable insights into how disruptions in cellular and immune processes can manifest as clinical symptoms.
Understanding the Role of Genes in Disease
The genetic basis of disease is a central theme in modern nursing research and medicine. Your analysis of Group A streptococcus pharyngitis in children and adolescents highlights an important aspect of pediatric health. This condition is often linked to an infection caused by the Group A streptococcus bacteria, but genetic predisposition also plays a crucial role in determining susceptibility and immune responses. The genetic factors that influence the body’s immune response to infection, such as the sensitivity of immune cells to bacterial toxins, are key to understanding why some individuals are more prone to recurrent infections than others. Studies suggest that genetic variations in the immune system’s response pathways may contribute to the frequency of Group A streptococcus infections (Centers for Disease Control and Prevention, 2021).
In nursing practice, understanding the genetic basis of disease is vital for creating effective care plans. For instance, recognizing the role of genetics in hypersensitivity reactions can help guide nursing assignments focused on patient education and identifying early signs of recurrent infections. This knowledge may also lead to more personalized treatment strategies for children with frequent sore throats or recurrent infections, integrating both genetics and immune system function into comprehensive care approaches.
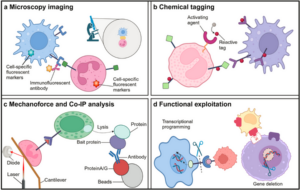
Cellular and Immune Response to Infection
The body’s defense system is activated when pathogens, such as bacteria or viruses, are recognized by the immune system. As you discussed, this triggers an inflammatory response that is often marked by symptoms such as a sore throat, fever, and swelling. The immune cells, including macrophages, T-cells, and B-cells, play pivotal roles in identifying and responding to antigens. The inflammatory pathway involves the release of various mediators like histamine and cytokines, which cause the classic signs of inflammation: heat, swelling, redness, and pain. These processes are well-documented in pathophysiology textbooks and highlight the complexity of the immune response in fighting infection.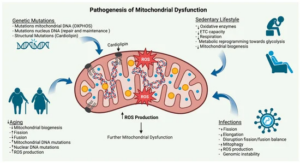
For nursing professionals, understanding these physiological processes is critical when diagnosing conditions like sore throat related to allergic conditions. Nurses often work to identify the underlying causes of symptoms, whether they stem from an infection, an allergic reaction, or another immune-mediated process. This is where nursing exams focused on differential diagnosis become crucial. For example, when assessing a patient presenting with a sore throat, nurses must consider both the infection-related and allergy-related causes, as these can require different management approaches.
Age and Immunity: A Key Factor in Disease Susceptibility
Age is a critical factor in how the immune system responds to disease. As noted, children are more susceptible to certain infections, such as Group A streptococcus pharyngitis, due to their developing immune systems. On the other hand, older adults often face an increased vulnerability to specific ailments due to immune system senescence, or the aging of immune cells, which impairs the body’s ability to respond effectively to infections and allergens. This dynamic underscores the intricate relationship between age and immunity.
The nursing implications of age-related immune changes are substantial. For example, older adults may have an increased risk of developing severe allergic reactions or infections due to weakened immune defenses. These insights are often incorporated into nursing care plans that focus on prevention and early detection of these issues, aiming to mitigate risks associated with aging and improve patient outcomes. Nurses are also critical in educating patients and caregivers about age-related vulnerabilities to both infections and allergies, which is an essential aspect of nursing research and practice.
Drug Allergies and Age: A Significant Consideration
Your observation regarding drug allergies correlating with age is an important consideration in clinical settings. Older individuals are often more likely to develop allergic reactions to medications, possibly due to changes in their immune response or polypharmacy (the use of multiple medications). This phenomenon requires special attention from nurses who must not only recognize allergic reactions but also manage and mitigate their impact on patient health. Additionally, nurses must be prepared to educate patients about the importance of providing a comprehensive medication history, particularly in elderly patients, to avoid complications related to drug allergies (Soderholm et al., 2018).
In clinical practice, nursing research and nursing assignments often involve studying these age-related patterns in drug allergies and developing best nursing practices for managing such cases. Nurses may use online nursing essays and nursing papers to access the latest research and guidelines on drug allergy management in different age groups.
Conclusion: Genetic and Cellular Mechanisms in Disease
In conclusion, your thoughtful analysis underscores the importance of understanding both the genetic and cellular mechanisms underlying disease. Genes play a significant role in shaping how the body responds to pathogens and allergens, and disruptions in normal cellular functions can lead to disease processes such as allergic reactions and infections. By integrating nursing research into clinical practice, nurses can enhance their understanding of these underlying mechanisms, ultimately improving patient care.
Your recognition of the age-related factors in immune responses further enriches the discussion on disease mechanisms, offering insights into how age influences disease susceptibility and immune system function. These insights are critical for developing effective nursing care plans tailored to the specific needs of patients across different life stages. As we continue to advance in the field of nursing, resources such as custom nursing papers, top nursing essays, and online nursing exams will help nurses stay up-to-date on the latest developments in disease pathophysiology and patient care strategies.
The thorough understanding of these complex processes, coupled with a commitment to evidence-based practice, enables nurses to deliver more effective and compassionate care, particularly for vulnerable populations such as children and the elderly. Your detailed analysis contributes to a deeper understanding of the intricate relationship between genetics, immune responses, and cellular functions, which is essential for advancing patient care and improving clinical outcomes.
References
Soderholm, A. T., Barnett, T. C., Sweet, M. J., & Walker, M. J. (2018). Group A streptococcal
pharyngitis: Immune responses involved in bacterial clearance and GAS‐associated immunopathology. Journal of leukocyte biology, 103(2), 193-213.
McCance, K. L. & Huether, S. E. (2019). Pathophysiology: The biologic basis for disease in
adults and children (8th ed.). Mosby/Elsevier.
Centers for Disease Control and Prevention. (2021, November 23). Pharyngitis (strep throat): Information for clinicians. Retrieved March 1, 2022, from https://www.cdc.gov/groupastrep/diseases-hcp/strep-throat.html
Kidney transplantation is an effective intervention for individuals grappling with end-stage renal disease. Unfortunately, some recipients encounter complications, notably kidney rejection. This paper delves into the rationale behind the manifestation of symptoms in a patient experiencing acute kidney transplant rejection, explores the genes associated with this rejection, and elucidates the process of immunosuppression.
Introduction: Understanding the Patient’s Symptoms and Pathophysiology
The patient presented a combination of concerning symptoms: weight gain, decreased urinary output, fatigue, and a fever of 101°F. These symptoms indicate a potential issue with kidney function, a critical component of fluid and electrolyte regulation in the body. Weight gain in this context is linked to fluid retention due to impaired renal function. Normally, kidneys play an essential role in filtering excess fluids and electrolytes from the body; however, when kidney function is compromised, the balance is disrupted, leading to fluid overload. This is one of the primary causes of weight gain in patients with renal dysfunction.
The decreased urinary output, or oliguria, further supports the suspicion of impaired renal function, as the kidneys are unable to filter and excrete waste products properly. Oliguria is commonly associated with kidney injury or dysfunction, and is often a red flag for acute kidney problems. The fatigue observed in the patient is likely due to the buildup of toxins, such as ammonia, which the kidneys would normally eliminate. When these toxins accumulate in the bloodstream due to poor kidney function, they contribute to symptoms like fatigue, poor concentration, and metabolic acidosis. Additionally, anemia is a frequent complication in patients with kidney disease, often caused by reduced production of erythropoietin, a hormone that stimulates red blood cell production.
The patient’s elevated temperature of 101°F is likely indicative of an infection, which is a common complication for individuals who have undergone kidney transplantation. Immunosuppression, a common side effect of transplant medications, weakens the body’s ability to fight infections, making these patients particularly vulnerable to bacterial or viral infections (Rauen et al., 2020). This chain of events — renal dysfunction, oliguria, toxin buildup, fatigue, anemia, and fever — paints a picture of a patient struggling with complex post-transplant complications, requiring careful nursing assessments and targeted interventions.
Genes Involved in Kidney Transplant Rejection
The genetic landscape of kidney transplant rejection is multifaceted, with multiple genes influencing the risk of graft failure and the body’s immune response to a transplanted kidney. Genetic studies have identified key genes that are involved in both the immunological process of rejection and the body’s response to immunosuppressive therapies.
Several genes are implicated in transplant rejection, including CYP2EI, CYP3A5, CTLA4, CXL8, and coagulation factors II and V, which are involved in immune cell signaling and inflammation. These genes influence the body’s immune response to the foreign tissue, either promoting or dampening rejection. The Forkhead box P3 gene, which is involved in the development of regulatory T-cells, plays a central role in maintaining immune tolerance and preventing excessive rejection responses. Interleukin genes, particularly interleukin-1 beta, interleukin-2, and their receptor subunits, are critical in modulating the immune system after transplantation. These cytokines help regulate inflammation but can also contribute to graft rejection if not appropriately balanced (Arnold et al., 2022; Spicer & Runkel, 2019).
The major histocompatibility complex (MHC) genes, responsible for antigen presentation, are also key players in the recognition of foreign tissue and the initiation of immune responses. Variations in these genes can impact the likelihood of transplant rejection and influence the selection of immunosuppressive medications. Understanding these genetic factors is crucial for healthcare providers in tailoring nursing care plans that address not only the immunosuppressive treatment but also the genetic predispositions that may affect each patient’s response to therapy.
For nursing research, this information is vital when considering genetic screening and the development of personalized approaches to post-transplant care. Genetic studies can guide decisions on the intensity of immunosuppressive therapy, potentially reducing the risk of rejection episodes and optimizing patient outcomes.
The Process of Immunosuppression in Kidney Transplant Recipients
Immunosuppression is a key component of the management of kidney transplant recipients. After a kidney transplant, patients are typically prescribed immunosuppressive medications to prevent the body from rejecting the new organ. These medications work by suppressing the immune system’s response to the transplanted kidney, effectively preventing the production of antibodies that would otherwise attack the graft. However, this suppression of the immune system comes at a significant cost: an increased risk of infections and cancer (Gupta et al., 2021).
In addition to the medications, some patients may experience drug-induced immunosuppression, which can occur when the body’s ability to process and metabolize the immunosuppressive drugs is impaired, often due to genetic polymorphisms. This leads to over-suppression of the immune system and greater susceptibility to infections. Nurses caring for kidney transplant recipients need to closely monitor for signs of infection, rejection, and adverse reactions to immunosuppressive therapy. Nursing assignments related to transplant care frequently involve ongoing assessments of immune function, laboratory results, and patient symptoms to ensure early detection of complications.
The consequences of immunosuppression are far-reaching, impacting patients’ daily lives and their overall health. The increased susceptibility to infections requires careful management, including patient education on infection prevention, the importance of hand hygiene, and timely medical intervention if signs of infection arise. Additionally, the financial burden of frequent hospital visits for infection treatment, as well as psychosocial stress, can further affect the patient’s quality of life. Nurses play a critical role in supporting these patients by providing holistic care that addresses not only the clinical aspects of transplant management but also the emotional and social challenges that come with living with a suppressed immune system.
Conclusion: The Interplay of Genetics, Kidney Transplant, and Immunosuppression
In conclusion, the patient’s symptoms of weight gain, oliguria, fatigue, and fever are directly related to the compromised renal function and the complex interplay of genetic and immunological factors following a kidney transplant. The genetic predispositions, especially those related to rejection pathways and immunosuppressive medication responses, underscore the importance of personalized care in kidney transplant recipients. Understanding the genetic underpinnings of transplant rejection allows nurses to make informed decisions regarding patient care, including adjustments in immunosuppressive therapy and more precise monitoring for complications such as infection or organ rejection.
For nursing practice, this information highlights the importance of integrating genetic knowledge into clinical decision-making and nursing care plans. Nurses must be equipped with up-to-date information from nursing research, including the latest insights from nursing papers, custom nursing papers, and online nursing essays, to provide the most effective care for kidney transplant patients. This knowledge is crucial in enhancing the patient’s quality of life and improving long-term outcomes by reducing the risk of rejection, infection, and other post-transplant complications.
References
Arnold, M.-L., Heinemann, F. M., Oesterreich, S., Wilde, B., Gäckler, A., Goldblatt, D., Spriewald, B. M., Horn, P. A., Witzke, O., & Lindemann, M. (2022). Correlation of Fc Receptor Polymorphisms with Pneumococcal Antibodies in Vaccinated Kidney Transplant Recipients. Vaccines, 10(5), Article 5. https://doi.org/10.3390/vaccines10050725
Gupta, R., Woo, K., & Yi, J. A. (2021). Epidemiology of end-stage kidney disease. Seminars in Vascular Surgery, 34(1), 71–78. https://doi.org/10.1053/j.semvascsurg.2021.02.010
Rauen, T., Wied, S., Fitzner, C., Eitner, F., Sommerer, C., Zeier, M., Otte, B., Panzer, U., Budde, K., Benck, U., Mertens, P. R., Kuhlmann, U., Witzke, O., Gross, O., Vielhauer, V., Mann, J. F. E., Hilgers, R.-D., Floege, J., Floege, J., … Hilgers, R.-D. (2020). After ten years of follow-up, no difference between supportive care plus immunosuppression and supportive care alone in IgA nephropathy. Kidney International, 98(4), 1044–1052. https://doi.org/10.1016/j.kint.2020.04.046
Spicer, P., & Runkel, L. (2019). Costimulatory pathway targets for autoimmune and inflammatory conditions: Clinical successes, failures, and hope for the future. Expert Opinion on Investigational Drugs, 28(2), 99–106. https://doi.org/10.1080/13543784.2019.1557146
van Vugt, L. K., Schagen, M. R., de Weerd, A., Reinders, M. E., de Winter, B. C., & Hesselink, D. A. (2022). Investigational drugs for the treatment of kidney transplant rejection. Expert Opinion on Investigational Drugs, 31(10), 1087–1100. https://doi.org/10.1080/13543784.2022.2130751

Dont wait until the last minute.
Provide your requirements and let our native nursing writers deliver your assignments ASAP.

