Diversity and Health Assessment Discussion week 2
 In this discussion, we will focus on Case Study 1, which revolves around John Green, a 33-year-old Caucasian male who identifies as a male but was assigned female at birth.
In this discussion, we will focus on Case Study 1, which revolves around John Green, a 33-year-old Caucasian male who identifies as a male but was assigned female at birth.
He transitioned from female to male two years ago, and he has recently moved back home and is currently unemployed.
John has a history of smoking two packs of cigarettes per day for the last decade, occasional marijuana use, and experiences depressive episodes.
He has been HIV-positive for three years but maintains viral suppression. Lately, he’s been feeling weak, which led to his decision to move back home and live with his parents. He takes medication for HIV and testosterone.
Diversity and Health Assessment Discussion Week 2 – Case Study 1
Let’s reflect on various factors related to John’s health, such as his socioeconomic status, spirituality, lifestyle, and cultural background. These aspects can significantly impact his health.

Struggling to meet your deadline?
Get your assignment on Diversity and Health Assessment Discussion week 2 done by certified MDs and PhDs in the USA. ORDER NOW!
To build a comprehensive health history for John, we need to approach it in a gender-affirming manner, ensuring that we use the right name and pronouns during the interview. This is vital to respect his identity (Ball. J, et al, 2019). Our physical examination should be sensitive to his existing anatomy without making assumptions about his identity. Considering the unique changes related to hormone therapy and surgical interventions is crucial.
Since Mr. J.G. is a transgender man, we should ask sensitive questions about his sexual partners and practices, as well as address potential issues related to domestic violence, which is more common among transgender individuals (Base & Nagy, “Cultural Competence in the Care of LGBTQ Patients”). Access to healthcare and financial concerns should also be discussed, along with an assessment of his support system since he returned home.
To collect pertinent information and assess his health risks, we could ask questions like:
1. How many sexual relationships have you had?
2. What is the gender of your sexual partners?
3. Are you currently sexually active?
4. Can you tell me when you were diagnosed with HIV?
5. What was your most recent CD4 count?
6. Have you used any illicit drugs?
When communicating with patients from diverse populations, it’s essential to be culturally sensitive. Strategies to achieve this as a nurse include:
– Developing cultural awareness and self-reflection to provide nonjudgmental and respectful patient-centered care.
– Informing patients about their conditions and involving them in their care decisions.
– Practicing cultural humility by respecting cultural differences and avoiding judgment.
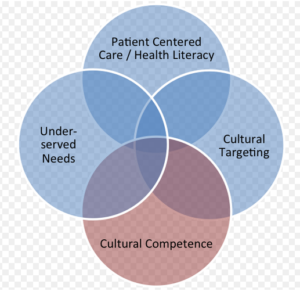
– Employing all dimensions of cultural competence, especially when caring for patients like John, whose diverse backgrounds can lead to stereotypes, judgments, or prejudices.
As a nurse practitioner, it’s our responsibility to offer quality care to all patients, regardless of their cultural, lifestyle, or health status differences, and to work collaboratively with them to address their concerns and make informed healthcare choices.
References
Ball, J. W., Dains, J. E., Flynn, J. A., Solomon, B. S., & Stewart, R. W. (2019). Seidel’s guide to physical examination: An Interprofessional Approach (9th ed.). St. Louis, MO: Elsevier Mosby.
Bass B, Nagy H. Cultural Competence in the Care of LGBTQ Patients. (Updated 2022 Oct 3). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Retrieve from: https://www.ncbi.nlm.nih.gov/books/NBK563176/ Diversity and Health Assessment Discussion week 2
Diversity and Health Assessment Discussion Week 2
Case Study Overview
In this discussion, we will focus on Case Study 1, which revolves around John Green, a 33-year-old Caucasian male. John identifies as male but was assigned female at birth. He transitioned from female to male two years ago and has recently moved back home. Currently unemployed, John has a history of smoking two packs of cigarettes daily for the last decade, occasional marijuana use, and experiences depressive episodes. He has been HIV-positive for three years but maintains viral suppression. Recently, he’s been feeling weak, which led him to move back home to live with his parents. John takes medication for HIV management and testosterone.
Health History Considerations
To build a comprehensive health history for John, we must approach it in a gender-affirming care manner. This means using the correct name and pronouns during the interview. Respecting John’s identity is crucial (Ball et al., 2019). Our physical examination should be sensitive to his anatomy, without making assumptions based on his gender identity.
As a transgender man, it’s important to ask sensitive questions about his sexual partners and practices. We should also address potential issues like domestic violence, which is more common among transgender individuals (Base & Nagy, 2022). Additionally, we need to consider socioeconomic factors in health, as John’s unemployment may affect his access to care and support systems.
To gather relevant information, we might ask questions such as:
- How many sexual relationships have you had?
- What is the gender of your sexual partners?
- Are you currently sexually active?
- Can you tell me when you were diagnosed with HIV?
- What was your most recent CD4 count?
- Have you used any illicit drugs?
These questions align with effective health assessment tools that can help us identify potential health risks.
Culturally Sensitive Communication Strategies
 When working with patients from diverse backgrounds, including LGBTQ+ healthcare, being culturally sensitive is essential. Here are some strategies:
When working with patients from diverse backgrounds, including LGBTQ+ healthcare, being culturally sensitive is essential. Here are some strategies:
- Developing cultural awareness: This involves self-reflection to provide care that is nonjudgmental and respectful.
- Patient-centered communication: Informing patients about their conditions and involving them in care decisions fosters trust and cooperation.
- Cultural humility: It’s important to respect cultural differences and avoid making judgments. This approach is crucial when caring for patients like John, whose identity may be affected by stereotypes or prejudices.
As a nurse practitioner, we have a responsibility to offer quality care to all patients, regardless of their cultural or health backgrounds. This includes understanding mental health and substance use issues, especially in individuals facing stigma or discrimination.
Ultimately, all dimensions of culturally competent care must be employed to help patients like John navigate their health journeys effectively.
References
Ball, J. W., Dains, J. E., Flynn, J. A., Solomon, B. S., & Stewart, R. W. (2019). Seidel’s guide to physical examination: An Interprofessional Approach (9th ed.). St. Louis, MO: Elsevier Mosby.
Bass, B., & Nagy, H. (2022). Cultural Competence in the Care of LGBTQ Patients. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK563176/

Dont wait until the last minute.
Provide your requirements and let our native nursing writers deliver your assignments ASAP.

